| Mycobacterium tuberculosis | |
|---|---|
 | |
| M. tuberculosis bacterial colonies | |
| Scientific classification | |
| Kingdom: | Bacteria |
| Phylum: | Actinobacteria |
| Order: | Actinomycetales |
| Suborder: | Corynebacterineae |
| Family: | Mycobacteriaceae |
| Genus: | Mycobacterium |
| Species: | M. tuberculosis |
| Binomial name | |
| Mycobacterium tuberculosis Zopf 1883 | |
| Synonyms | |
| Tubercle bacillus Koch 1882 | |
Mycobacterium tuberculosis (MTB) is a pathogenic bacterial specie in the genus Mycobacterium and the causative agent of most cases of tuberculosis.[1] First discovered in 1882 by Robert Koch, M. tuberculosis has an unusual, waxy coating on the cell surface (primarily mycolic acid), which makes the cells impervious to Gram staining so acid-fast detection techniques are used instead. The physiology of M. tuberculosis is highly aerobic and requires high levels of oxygen. Primarily a pathogen of the mammalian respiratory system, MTB infects the lungs and is the causative agent of tuberculosis.The most frequently used diagnostic methods for TB are the tuberculin skin test, acid-fast stain, and chest radiographs.[1]
The M. tuberculosis genome was sequenced in 1998.[2][3]
Pathophysiology
M. tuberculosis requires oxygen to grow. It does not retain any bacteriological stain due to high lipid content in its wall, and thus is neither Gram positive nor Gram negative; hence Ziehl-Neelsen staining, or acid-fast staining, is used. While Mycobacteria do not seem to fit the Gram-positive category from an empirical standpoint (i.e., they do not retain the crystal violet stain), they are classified as acid-fast Gram-positive bacteria due to their lack of an outer cell membrane.[1]
M. tuberculosis divides every 15–20 hours, which is extremely slow compared to other bacteria, which tend to have division times measured in minutes (Escherichia coli (E. coli) can divide roughly every 20 minutes). It is a small bacillus that can withstand weak disinfectants and can survive in a dry state for weeks. Its unusual cell wall, rich in lipids (e.g., mycolic acid), is likely responsible for this resistance and is a key virulence factor.[4]
When in the lungs, M. tuberculosis is taken up by alveolar macrophages, but they are unable to digest the bacterium. Its cell wall prevents the fusion of the phagosome with a lysosome. Specifically, M. tuberculosis blocks the bridging molecule, early endosomal autoantigen 1 (EEA1); however, this blockade does not prevent fusion of vesicles filled with nutrients. Consequently, the bacteria multiply unchecked within the macrophage. The bacteria also carried the UreC gene, which prevents acidification of the phagosome.[5] The bacteria also evade macrophage-killing by neutralizing reactive nitrogen intermediates.
The ability to construct M. tuberculosis mutants and test individual gene products for specific functions has significantly advanced our understanding of the pathogenesis and virulence factors of M. tuberculosis. Many secreted and exported proteins are known to be important in pathogenesis.[6]
Strain Variation
M. tuberculosis Comes from the genus Mycobacterium,which is composed of approximately 100 recognized and proposed species. The most familiar of the species are Mycobacterium tuberculosis and Mycobacterium leprae(Leprosy)(Page 576;Textbook of Diagnostic Microbiology, Mahon, Lehman, Manuselis). M. tuberculosis appears to be genetically diverse. A genetic diversity results in significant phenotypic differences between clinical isolates. M. tuberculosis exhibits a biogeographic population structure and different strain lineages are associated with different geographic regions. Phenotypic studies suggest that this strain variation never has implications for the development of new diagnostics and vaccines. Micro-evolutionary variation affects the relative fitness and transmission dynamics of antibiotic-resistant strains.[7]
Hypervirulent Strains
Mycobacterium outbreaks are often caused by hypervirulent strains of M. tuberculosis. In laboratory experiments, these clinical isolates elicit unusual immunopathology and may be either hyperinflammatory or hypoinflammatory. Studies have shown that the majority of hypervirulent mutants have deletions in their cell wall modifying enzymes or regulators that respond to environmental stimuli. Studies of these mutants have indicated the mechanisms that enable M. tuberculosis to mask its full pathogenic potential, inducing a granuloma that provides a protective niche and enables the bacilli to sustain a long-term persistent infection.[8]
Microscopy
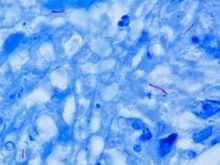
M. tuberculosis is characterized by caseating granulomas containing Langhans giant cells, which have a "horseshoe" pattern of nuclei. Organisms are identified by their red color on acid-fast staining.
Genome
The genome of the H37Rv strain was published in 1998.[9] Its size is 4 million base pairs, with 3959 genes. 40% of these genes have had their function characterised, with possible function postulated for another 44%. Within the genome are also 6 pseudogenes.
The genome contains 250 genes involved in fatty acid metabolism, with 39 of these involved in the polyketide metabolism generating the waxy coat. Such large numbers of conserved genes shows the evolutionary importance of the waxy coat to pathogen survival.
10% of the coding capacity is taken up by 2 clustered gene families that encode acidic glycine rich proteins. These proteins have a conserved N-terminal motif, deletion of which impairs growth in macrophages and granulomas.[10]
Nine non-coding sRNAs have been characterised in M. tuberculosis[11] with a further 56 predicted in a bioinformatics screen.[12]
Symptoms
It is estimated that only about 10% of people infected with M. tuberculosis ever develop tuberculosis disease and many of those have the disease only for the first few years following infection even though the bacillus may lie dormant in the body for decades.[13]
The symptoms that patients infected with M. tuberculosis may experience are usually absent until the disease has become more complicated. It may take many months from the time the infection initially gets into the lungs until symptoms develop.[14] Cough is however the first symptom of the infection with M. tuberculosis.[15] The initial symptoms, including loss of appetite, fever, productive cough and loss of energy or loss of weight or night sweats are not specific and might be easily attributed to another condition.
Primary pulmonary tuberculosis is the first stage of the condition and it may cause fever, dry cough and some abnormalities that may be noticed on a chest x-ray. However, in most cases, primary infections tend to cause no symptoms that people do not overcome. This condition resolves itself although it returns in more than half cases.
Tuberculosis causing lung disease may result in tuberculous pleuritis, a condition that may cause symptoms such as chest pain, nonproductive cough and fever. Moreover, infection with M. tuberculosis can spread to other parts of the body, especially in patients with a weakened immune system. This condition is referred to as miliary tuberculosis and people contacting it may experience fever, weight loss, weakness and a poor appetite. In more rare cases, miliary tuberculosis can cause cough and difficulty breathing.
Dormant (inactive) tuberculosis may return after a certain period of time and it usually occurs in the upper lungs causing severe symptoms such as common cough with a progressive increase in production of mucus and coughing up blood.[13] Most patients also develop fever, loss of appetite, unexplained weight loss and night sweats.
In cases in which the infection spreads to other parts of the body, additional symptoms may occur, depending on the exact site of the spread. If the infection spreads to the abdominal cavity, symptoms such as fatigue, swelling, slight tenderness and appendicitis-like pain are likely to occur. Also, painful urination might be a sign that the infection has reached the bladder. In children, M. tuberculosis infections may affect the bones causing mild swelling and minimal pain. Fever, headache, nausea, drowsiness, and, if untreated, coma and brain damage may occur if the brain has been affected.[15] If the infection affects the pericardium, symptoms and signs such as fever, enlarged neck veins, and shortness of breath may develop. Kidney damage and the symptoms emerging with it as well as sterility may occur if the kidney, respectively the reproductive system are affected.
Diagnosis
Sputum is taken on three successive mornings as the number of organisms could be low, and the specimen is treated with 3% KOH or NaOH for liquefaction and decontamination. Gram stain should never be performed, as the organism is an "acid-fast bacillus" (AFB), meaning that it retains certain stains after being treated with acidic solution. In the most common staining technique, the Ziehl-Neelsen stain, AFB are stained a bright red, which stands out clearly against a blue background; therefore, the bacteria are sometimes called red snappers.[16] The reason for the acid-fast staining is because of its thick waxy cell wall.[17] The waxy quality of the cell wall is mainly due to the presence of mycolic acids. This waxy cell wall also is responsible for the typical caseous granuloma formation in tuberculosis. The component responsible, trehalose dimycolate, is called the cord factor. A grading system exists for interpretation of the microscopic findings based on the number of organisms observed in each field. Patients of pulmonary tuberculosis show AFB (acid fast bacillus) in their sputum in only 50% of cases, which means that, even if no organisms are observed, further investigation is still required. Acid-fast bacilli can also be visualized by fluorescent microscopy using auramine-rhodamine stain for screening, which makes them appear somewhat golden in color. Also, M. tuberculosis is grown on a selective medium known as Lowenstein-Jensen medium, which has traditionally been used for this purpose. However, this method is quite slow, as this organism requires 6–8 weeks to grow, which delays reporting of results. A faster result can now be obtained using Middlebrook medium or BACTEC.
It should be taken into consideration that during an advanced stage of tuberculosis, the organism may infect almost any part of the body, which means that a specimen should appropriately be chosen (e.g. intestinal tuberculosis-stool).
An immunochromatographic serological essay for the diagnosis of M. tuberculosis has also been developed.[18]
Treatment
Treatment is usually administered on an outpatient basis and it consists mainly of medication. Usually, the treatment is given for six to nine months according to a therapy regimen consisting of two months of isoniazid, rifampin, and pyrazinamide, four months of isoniazid and rifampin and ethambutol or streptomycin until the drug sensitivity is known.[19] The drug treatment schema may be changed according to the laboratory results.
Antibiotics are usually part of therapy in people who have no symptoms and whose germs are in inactive state. Antibiotics in this case are helpful in preventing the activation of the infection. The antibiotic used for this purpose is called isoniazid (INH). If taken for six to 12 months, it will prevent the tuberculosis from becoming active in the future.[20] This medicine may not however be taken during pregnancy or in people who suffer from liver disease or alcoholism. Moreover, several side effects have been reported to this drug and some of them can be even life-threatening. One of the side effects caused by this drug is peripheral neuropathy, meaning a decreased sensation in the extremities and which is normally prevented or avoided by administering vitamin B6 at the same time with isoniazid.
Patients who have active bacteria are usually treated with a combination of medications, at the same time with the main antibiotic, isoniazid. The main drugs used in conjunction with isoniazid are rifampin, ethambutol and pyrazinamide.
Streptomycin, a drug that is given by injection, may be used as well, particularly when the disease is extensive and/or the patients do not take their oral medications reliably (termed "poor compliance").[20]
Usually treatment lasts for few months but it can even be administered for years, in some cases. Mainly, the rate of success of the treatment is in close relation with the patient's compliance and ability to take the drugs as prescribed.
History
M. tuberculosis, then known as the tubercle bacillus, was first described on 24 March 1882 by Robert Koch, who subsequently received the Nobel Prize in physiology or medicine for this discovery in 1905; the bacterium is also known as Koch's bacillus.[21]
Infections with tuberculosis have always been existent although their names have constantly changed over the time. However, it is not until 1720 that the history of tuberculosis starts to take shape into what is known of it today as the physician Benjamin Marten describes in his A Theory of Consumption that tuberculosis may be caused by small living creatures that are transmitted through the air to other patients.[22]
No comments:
Post a Comment